September 20, 2022
This blog was originally posted the American Society on Aging website on September 19 in recognition of Malnutrition Awareness Week, September 19-23, 2022.
Food insecurity and malnutrition can contribute to health disparities as poor diet and lack of access to healthy foods drive health inequities. Malnutrition Awareness Week, September 19–23, 2022, is a prime opportunity to raise awareness about the more than 34.8 million people living in U.S. households struggling to put food on the table. While not everyone who is food insecure is malnourished or vice versa, food insecurity and malnutrition are related conditions that impact tens of millions of people. The term food insecurity means a household-level economic and social condition of limited or uncertain access to adequate food, and malnutrition is considered a state of deficit, excess or imbalance in protein, energy or other nutrients that adversely affects an individual’s body form, function and clinical outcomes.
With up to 50% of older adults at risk of becoming or already malnourished, and millions of older adults experiencing food insecurity, there is a large, unmet need that can be reduced through improved education of health providers on the overlap of food insecurity and malnutrition, and on the importance of connecting patients to federal nutrition programs such as the U.S. Department of Agriculture (USDA) Supplemental Nutrition Assistance Program (SNAP, formerly known as Food Stamps).
The 2021 food insecurity rate of 7.1% among households with older adults (ages 65 and older) is surprisingly lower than the 2020 national average of 10.2% in large part because of the importance of Social Security and Medicare in reducing poverty among older adults. Additionally, at ages 60 or older, adults are eligible for programs such as home-delivered meals and congregate meals and can benefit from SNAP policies that streamline access and allow applicants to claim additional deductions such as medical and uncapped excess housing costs.
Connecting older adults to SNAP is a winning strategy to address both food insecurity and malnutrition. A considerable body of evidence supports the critical role of SNAP in improving the food security and physical and mental health of older adults. Unfortunately, too few older adults are enrolled in these programs. In 2018, only 48% of eligible older adults participated in SNAP.
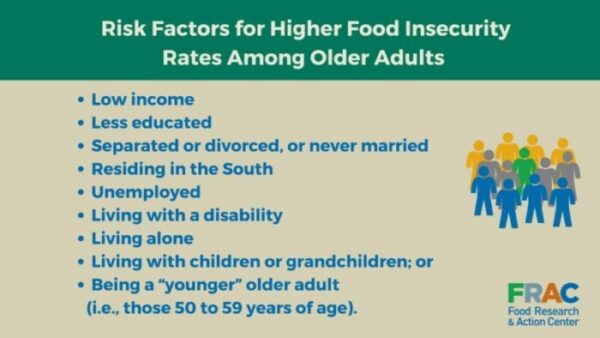
Even with lower overall rates of food insecurity, certain groups of older adults struggle with higher rates. This is largely driven by poverty and other factors like household composition, as indicated in the graphic below. Parents, grandparents and other caregivers often try to protect children from food insecurity by sacrificing their own food and nutrition needs so that the children can eat. Fueled by underlying structural discrimination and other inequities, food insecurity rates are disproportionately higher for Black, Latinx and other older adult households of color compared to White households. Rates among adults ages 65 and older living alone increased from 2020–2021 (from 8.3% to 9.5%), the highest rate in 20 years. This could be due to older adults’ fixed incomes not keeping pace with inflation and expanded federal programs, such as the Child Tax Credit, not reaching adults living alone.
Figure 1, below, shows risk factors for food insecurity for older adults.
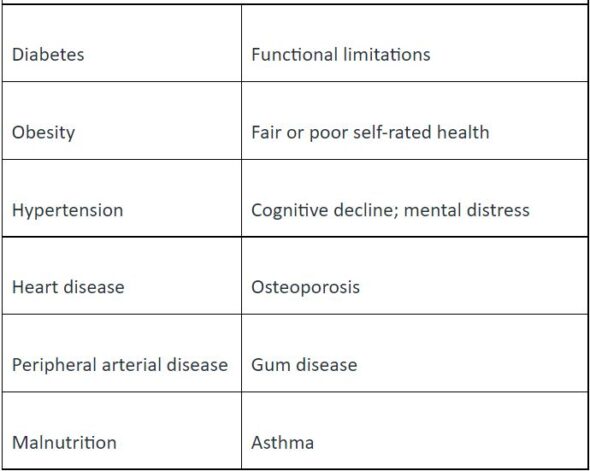
Food insecurity fuels some of our nation’s most chronic, serious and costly health conditions. As shown in Figure 2, below, adults experiencing food insecurity face many health challenges that can be exacerbated by coping strategies such as forgoing medical care and medication to pay for food. Among adults, food insecurity or its associated health-compromising coping strategies are at odds with healthy aging because they can exacerbate existing diseases and compromise health. This can result in, for example, poor glycemic control or end-stage renal disease. It can also:
- increase physician encounters and office visits,
- increase emergency room visits, and
- increase hospitalizations.
Figure 2, below, details conditions related to food insecurity in older adults.
Physical and Mental Health Consequences Associated With Food Insecurity Among Older Adults
Food insecurity and malnutrition are interconnected conditions, with food insecure older adults having lower nutrient intakes. Malnutrition can have deleterious effects on older adult health, especially when other conditions are present. Unfortunately, malnutrition is not frequently identified or treated, but it is preventable. Healthcare professionals and others caring for at risk older adults need tools and information to identify those in need and educate them on resources available to help purchase or otherwise access nutritious food. With effective tools, food insecurity and malnutrition can be better identified and addressed, leading to improved health outcomes.
In recognition of Malnutrition Awareness Week, get involved by learning more about food insecurity and its connections to malnutrition. Here are great resources to get you started:
- Take this free, one-hour, online course: Screen & Intervene: Addressing Food Insecurity Among Older Adults. The Food Research & Action Center, in collaboration with AARP Foundation, designed this course to help frontline health workers and others identify and address food insecurity by connecting older adults to nutrition resources like SNAP to improve their nutrition, health and well-being. Participants are eligible to receive one Continuing Medical Education (CME) credit.
- Participate in an improvement activity. The Centers for Medicare & Medicaid Services recognized the importance of food insecurity and nutrition risk in impacting health outcomes and equity by including a food insecurity and nutrition risk improvement activity for office-based physicians and clinicians who participate in the Merit-Based Incentive Payment System starting in 2022. Integrating quality nutrition care into this framework can help to better address chronic diseases and support active aging. For more information, visit the Malnutrition Quality Improvement Initiative.
Alexandra Ashbrook, JD, LLM, is the director of Root Causes and Specific Populations at Food Research & Action Center. Laura Borth, MS, RD, is a policy associate at Defeat Malnutrition Today.

