Published August 15, 2025
Food insecurity takes a toll on maternal, infant, and child health.
In 2023, 47.4 million people — including 13.8 million children — lived in food-insecure households.
Food insecurity is linked to poor health and development and is associated with some of the most common and costly health problems in the U.S. For adults and pregnant women, its linked to fair or poor health status, pregnancy complications (e.g., gestational diabetes, iron deficiency), and depression (including maternal depression). For infants and children, food insecurity is especially detrimental to health, development, and well-being, with links to low birth weight, birth defects, more frequent colds and stomachaches, development risk, increased hospitalizations, and more.
But it doesn’t need to be this way.
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is a proven intervention for improving health, food security, and economic security, and generating other positive outcomes.
WIC provides pregnant, postpartum, and breastfeeding individuals, infants, and children up to 5 years of age from households with low incomes with nutritious foods, education and counseling, and referrals to health care and social services. Receiving WIC improves perinatal and maternal health outcomes and helps ensure that children have good nutrition to support key development milestones in the critical early years.
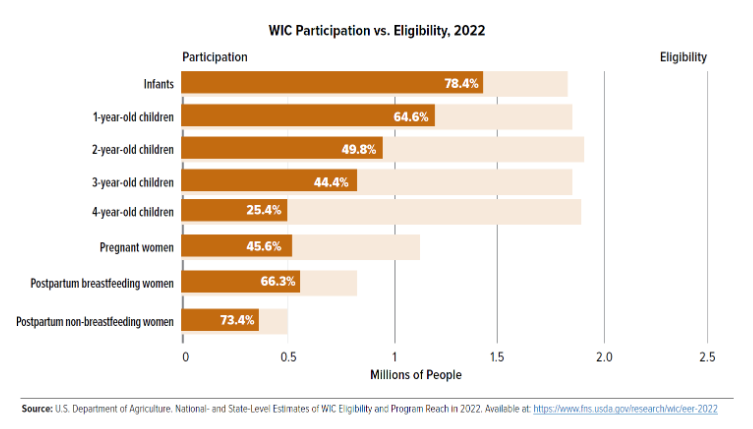
Despite the substantial benefits of WIC, far too many eligible people are not participating in the program.
Nationally, nearly 5.5 million eligible people missed out on WIC’s support in 2022, with especially low coverage rates (all eligible people compared to those participating) among children and pregnant women.
Health care providers can leverage WIC to improve health.
Connecting eligible people to WIC is an evidence-based strategy to address the nutrition and health issues linked to food insecurity, and health care providers have an essential role in helping boost WIC access among their patients.
A new toolkit produced by FRAC in partnership with Drs. Kofi Essel and Kimberly Montez helps health care providers, medical professionals, and anyone who treats or engages with families learn about opportunities to begin or ramp up work to connect patients and families to WIC.
The toolkit provides key topline information on WIC to help those newer to the program, or those who could use a refresher, get oriented to WIC basics. It also has a companion piece that provides a deeper dive into the program.
The toolkit focuses on four key steps for providers to integrate WIC into their practice:
Included for each of the four steps are examples of different ways to carry out the work so that providers get a sense of available options, as well as factors to consider when figuring out the strategies that are right for their setting and patients. For example, the toolkit lifts up ideas on early work to establish partnerships with WIC clinics and anti-hunger organizations, how to learn about WIC policies and procedures, the importance of identifying champions to lead this work in their setting, and training staff. There are also features that showcase how states and health care providers or practices are making connections to WIC.
The toolkit highlights how there are many different ways health care providers can integrate WIC into their work with patients, depending on factors like capacity, workflow, and partnerships. The key is to get started, no matter how big or small the steps, and to grow the work over time. Each connection to WIC helps to build the foundation for a strong, healthy future.
Check out the toolkit, Connecting Families to WIC: A Practical Toolkit for Health Care Providers, and the associated webinar recording to learn more. Share the toolkit with health care provider partners in your network. https://ctt.ec/Gc4U1

